Engender blog
Guest Post: Contraception information and consent - two sides of the same coin?
As discussions around schemes which offer women support on the condition they utilise long-acting reversible contraceptives (LARC) continue, we'll be hosting a series of blogs by Elspeth Wilson discussing her research into how LARC has historically been - and continues to be - used to control the fertility of marginalised people. Read Elspeth's previous blog here.
In her second blog, Elspeth discusses ideas around informed consent.
-400.png)
"… they did not mention any of the side-effects nor provide any kind of informational material about what the injection does." [quote from research participant]
Many of the women I spoke to mentioned speaking to peers and older women to get the kind of advice on contraception that they wanted, but some researchers have queried the accuracy of peer-to-peer advice and looked for ways to encourage a focus on medical guidance instead (Okpo et al, 2014). However, this approach assumes that people can get everything they need from medical sources which, in reality, is not always the case. An American study found that doctors sometimes downplay or omit to mention the possibility of side-effects in consultations with patients, to the point that scientific evidence on LARC was sometimes contradicted (Littlejohn and Kimport, 2017). Whilst similar research in the UK would be useful, this study suggests that clinicians can construct knowledge in ways that may differ from those with lived experience of LARC. British research suggests that GPs sometimes have outdated knowledge about LARC with many believing that the coil is not suitable for people in their teens and twenties, thinking that it can cause infertility (Middleton et al, 2011).
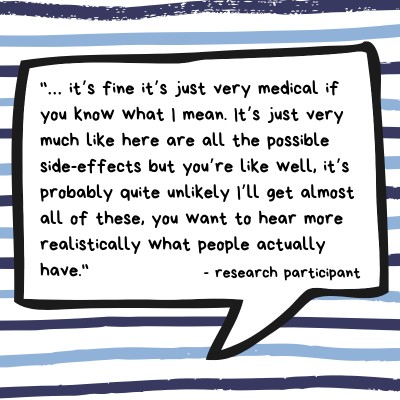
Of the women I spoke to, those who got their information about contraception from a variety of sources – including but not limited to medical advice – had the best experience. This might have been because these participants were largely affluent so less likely to suffer from health inequalities and adverse outcomes anyway. More research is required in this area (as is so often the case in women’s health) but it is worth considering that it was the most advantaged women who had the most sources of support and information available to them; where does this leave those who are already more likely to experience health inequalities?
Many women value learning about others’ experiences as well as clinical knowledge. For my research participants, friends and sometimes family provided feminine support and knowledge networks to those who had not been able to find the information they wanted elsewhere. Whilst there is no such thing as a homogenous ‘women’s perspective’, lived experiences can provide ways of knowing that are often missing from mainstream discourse where sources of knowledge are usually men.
And it is no wonder that people want to find out as much information as possible; a lack of information can have devastating consequences for women. One participant hadn’t been told to check the location of her implant so was unconcerned when she couldn’t feel it in her arm until the time came to have it removed.
"When I visited the doctor and explained that I thought removal could be difficult as I couldn’t feel it within my arm. The doctor I visited agreed and asked why I hadn’t reported that I couldn’t feel the implant in my arm before this. This was something I had never been informed of when getting an implant inserted although I have since learned that it is supposed to be common practice now to alert everyone to this possibility before insertion as technically without this information being given, consent and understanding have not been given."
Although she was initially dismissed and told that it was “physically impossible” for the implant to have travelled, it was eventually located in her lung.
Whilst this is obviously a very rare case, it has wider applicability as it could have been avoided if the correct information was provided at the time of insertion. As she rightly pointed out, the fact that she wasn’t told routine information made the idea of ‘informed consent’ an impossibility. Several other participants felt that they had been given inaccurate or misleading advice, such as not being given any information about the potentially delayed onset of ovulation after stopping using the injection. Real consent can only be given when a patient is making an informed choice. To improve consent in contraceptive care it is vital that patients are able to get the most accurate information possible before making a decision.

Who is given what advice – or lack thereof – is also a crucial consideration given racist, ableist and classist histories of reproductive control and coercion. Several women in their late teens and early twenties who I spoke to believed that doctors didn’t tell them about the time it can take to conceive after using the injection because of their youth and continued to dismiss their concerns because of this after they experienced problems getting pregnant. In America, researchers found that when shown a video of 27-year-old women from different socioeconomic groups and races, doctors were more likely to recommend a coil to low-income women of colour than low-income white women, showing how oppression can intersect in clinical advice (Dehlendorf et al, 2010). For women from marginalised groups, talking to peers may well provide information about contraception that they are unlikely to get elsewhere.
With the arrival of the Pause programme in Scotland, which requires vulnerable women to use long-acting contraception to be able to access holistic help, a nuanced look at consent in contraception is overdue as is the consideration of what kind of guidance is on offer to those who already have their fertility devalued by society and medicine. A different way forward is possible where clinicians’ knowledge and patients’ knowledge can both be valued, and the presumptions and biases that shape advice on reproductive health addressed. Patients know above anyone else what they value in a contraceptive method. This should be recognised and combined with medical expertise so that patients are supported in choosing the right contraception for them regardless of their identity. I understand concerns that too great a focus on side-effects, many of which are relatively rare, may put off people from a contraception that they might get on with before they’ve even had a chance to try it. However, this gives women little credit. I wish I'd been told the IUD can contribute to vaginal infections and, ironically, might have stuck with it for longer if I'd been prepared and been able to be proactive. Greater knowledge will only ever allow people accessing contraception more freedom. Knowledge is power and in this case it is power and control over one’s own body.
References
Dehlendorf, Christine, Ruskin, Rachel, Grumbach, Kevin, Vittinghoff, Eric, BibbinsDomingo, Kirsten, Schillinger, Dean, Steinauer, Jody E. 2010. ‘Recommendations for intrauterine contraception: a randomized trial of the effects of patients' race/ethnicity and socioeconomic status.’ American Journal of Obstetrics and Gynaecology 203(4): 319.e1-319.e8.
Littlejohn, Krystale E., and Kimport Katrina. 2017. ‘Contesting and Differentially Constructing Uncertainty: Negotiations of Contraceptive Use in the Clinical Encounter’. Journal of Health and Social Behavior. 58(4): 442-454.
Middleton, Annie J., Naish, Jeanette and Singer, Nicola. 2011. ‘General practitioners' views on the use of the levonorgestrel-releasing intrauterine system in young, nulligravid women, in London, UK.’ The European Journal of Contraception & Reproductive Health Care 16(4): 311-318.
Okpo, Emmanuel, Allerton, Lisa, and Brechin, Sue. 2014. ‘‘But you can't reverse a hysterectomy!’ Perceptions of long acting reversible contraception (LARC) among young women aged 16–24 years: a qualitative study’. Public Health 128(10):934-939.
Elspeth is a researcher and writer with a focus on public health, medical anthropology and gender. Originally trained in social anthropology, she recently completed her MPhil in Gender Studies at Trinity College Dublin. She is currently working on a project about the experience of pleasure post-trauma and is always looking for creative, interdisciplinary ways to approach research. You can find her @ellijwilson and @propleasurable.
Guest posts do not necessarily reflect the views of Engender, and all language used is the author's own. Bloggers have received some editorial support from Engender, and may have received a fee from our commissioning pot. We aim for our blog to reflect a range of feminist viewpoints, and offer a commissioning pot to ensure that women do not have to offer their time or words for free.
Interested in writing for the Engender blog? Find out more here.
Share this post on …
Comments: 0 (Add)
Downloads
 Access to Abortion: Situating Scotland in the Western World
This paper describes the different legal and regulatory contexts for abortion healthcare in Scotland and in other European and western nations.
Access to Abortion: Situating Scotland in the Western World
This paper describes the different legal and regulatory contexts for abortion healthcare in Scotland and in other European and western nations.
 Our bodies our rights - Identifying and removing barriers to disabled women's reproductive rights in Scotland
Since 2013, Engender has been working with disabled women and disabled people’s organisations on a project to discuss the key issues facing women and girls in Scotland, and to enable a deeper and richer conversation about reproductive rights.
Our bodies our rights - Identifying and removing barriers to disabled women's reproductive rights in Scotland
Since 2013, Engender has been working with disabled women and disabled people’s organisations on a project to discuss the key issues facing women and girls in Scotland, and to enable a deeper and richer conversation about reproductive rights.
 Our Bodies, Our Choice: The Case for a Scottish Approach to Abortion
The devolution of abortion law as part of the Scotland Act 2016 also provides Scotland with the opportunity to develop a Scottish approach to women’s reproductive rights, incorporating improved, modernised and standardised service provision underpinned by a progressive devolved legal framework.
Our Bodies, Our Choice: The Case for a Scottish Approach to Abortion
The devolution of abortion law as part of the Scotland Act 2016 also provides Scotland with the opportunity to develop a Scottish approach to women’s reproductive rights, incorporating improved, modernised and standardised service provision underpinned by a progressive devolved legal framework.
 Our Bodies, Our Rights Easy Read Report
This is an Easy Read version of our Disabled Women: Our Bodies, Our Rights Report.
Our Bodies, Our Rights Easy Read Report
This is an Easy Read version of our Disabled Women: Our Bodies, Our Rights Report.
 Our Bodies, Our Rights: Research Report
Disabled women’s lives and lived experiences have received limited policy attention in the UK, limited visibility, and limited inclusion in mainstream feminisms and feminist projects.
Our Bodies, Our Rights: Research Report
Disabled women’s lives and lived experiences have received limited policy attention in the UK, limited visibility, and limited inclusion in mainstream feminisms and feminist projects.

Newsletter
Sign up to receive our newsletter here:
Sign up to our mailing list
Receive key feminist updates direct to your inbox: